Medicaid and CHIP are a lifeline for many low-income Americans, providing health care coverage when they need it most. However, enrollment in Medicaid and CHIP – unlike private insurance or Medicare – is like a sieve; every year millions of people enroll, only to subsequently lose their coverage, despite still being eligible. These interruptions in coverage, widely known as "churn," harm the continuity and effectiveness of care.
Representatives Gene Green and Joe Barton have introduced the bipartisan H.R. 2628, The Stabilize Medicaid and CHIP Coverage Act of 2017. Senator Sherrod Brown has introduced similar legislation, S. 1227, in the Senate. These bills provide 12-month continuous eligibility for all Medicaid and CHIP enrollees.
Urge your Members of Congress to cosponsor these important pieces of legislation, and add your organization's name to the list of supporters by contacting Jenny Babcock at ACAP.
|
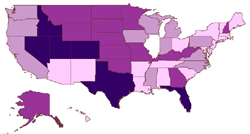
The Average Medicaid Enrollee Is In the Program 9.7 Months of the Year
|
Currently, the average Medicaid enrollee is on the program less than 10 months per year – see how your state compares. While some enrollees leave the Medicaid program owing to rising incomes, many are instead "churned": disenrolled and reenrolled in the program owing to bureaucratic and paperwork problems, or because they had a couple of extra hours of overtime in a week.
The Stabilize Medicaid and CHIP Coverage Act would reduce the number of low-income Americans who lack health insurance coverage and improve the stability, continuity and quality of care they receive. It will ensure more efficient and cost-effective care, both from the perspective of medical and administrative expenses.
For more information about how unstable coverage affects the millions of Americans who rely on Medicaid and CHIP, review the churn FAQs.